Share
 When the COVID-19 pandemic hit New York in March, most in-person services for people with intellectual and developmental disabilities (I/DD) disappeared overnight. This put many people at risk for losing years of hard-won progress in education, socialization, and crucial life skills. Destiny Lewis had received physical and occupational therapy for nearly two decades, but she quickly experienced challenges when the pandemic caused an interruption in traditional therapy. But within a week of shutting down these programs, YAI’s team of physical and occupational therapists were hard at work creating remote PT and OT plans that would not only help people with I/DD maintain progress but also increase their overall quality of care.
When the COVID-19 pandemic hit New York in March, most in-person services for people with intellectual and developmental disabilities (I/DD) disappeared overnight. This put many people at risk for losing years of hard-won progress in education, socialization, and crucial life skills. Destiny Lewis had received physical and occupational therapy for nearly two decades, but she quickly experienced challenges when the pandemic caused an interruption in traditional therapy. But within a week of shutting down these programs, YAI’s team of physical and occupational therapists were hard at work creating remote PT and OT plans that would not only help people with I/DD maintain progress but also increase their overall quality of care.
For Lewis and her mother Rebecca, the remote PT and OT program couldn’t be implemented soon enough. Lewis had been working with Abigail Tayamen Macatangay, Director of Rehabilitation Services at YAI, since 2003. Given the new stresses of the pandemic, Lewis became irritable and even refused to get out of bed. This pilot program helped Lewis when her mother felt things were taking a turn for the worse.
“We knew that if we didn’t fulfill the need and provide these services, the people we support would regress,” explained Macatangay. “We had to be creative and develop individualized experiences and different functional activities exclusive to each person we supported.”
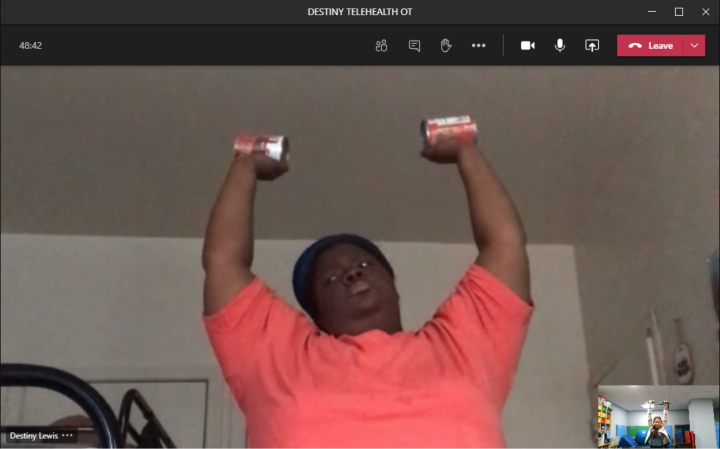
This included utilizing household items that were immediately available such as canned tomatoes or pasta sauce as makeshift weights to increase muscle mass. Macatangay said, “we would designate it as the official weight for them, but then, guess what--by the next session, it would be eaten!”
Each day brought new challenges, but one thing was consistent for Destiny Lewis: Macatangay’s virtual presence.
“Abby was calling and checking on us every day,” Lewis said. “It was wonderful, and it distracted Destiny from what was happening around her.”
 The remote program’s success initially hinged on one important denominator: comfort with the service provider. Its first iteration was rolled out to people who had already been receiving services from YAI’s Article 16 clinics, Premier HealthCare and YAI Center for Specialty Therapy (CST). Fortunately, both clinics were certified to provide telehealth services a few weeks before social distancing protocols were implemented globally.
The remote program’s success initially hinged on one important denominator: comfort with the service provider. Its first iteration was rolled out to people who had already been receiving services from YAI’s Article 16 clinics, Premier HealthCare and YAI Center for Specialty Therapy (CST). Fortunately, both clinics were certified to provide telehealth services a few weeks before social distancing protocols were implemented globally.
“We are educating staff or parents in the home on how to handle the situation, providing them with an understanding of how to fulfill needs that usually require being certified for a specific skill,” said Kristi Hickey-Vigilante, Director of Clinical, Family, and Community Services at YAI. “Education and coordination are major parts of it, but we have seen that the overall care provided to the people we support has improved.”
When word of the program’s success spread throughout YAI, staff approached Hickey-Vigilante with the desire to implement this system in YAI residences. However, many residents hadn’t received services from CST or Premier HealthCare before.
“We initially had to establish a baseline for each new patient, which required me, in full PPE gear, conducting an in-person evaluation,” Macatangay said. “We coordinated with staff to ensure not only the safety of the person we were looking to support but also our own staff members. Eventually, when staff would see how we interacted, it would prompt discussion on how to better work with that person.”
For many of the YAI residents that CST began treating, the benefits were immediately clear. The program staff could make sense of issues from a clinical perspective through advising from Macatangay.
“It informs the care, and these knowledge sessions became a part of staff training goals for work in each particular location,” Macatangay said. “We would tweak and evaluate plans in real time through multiple in-person sessions to establish a baseline. From there, we would transition to telehealth.”
Providing PT and OT remotely remains a relatively new area for YAI and its success is determined by communication and coordination on the part of therapists, staff, family members, and people receiving services. Although it may not be feasible for every situation, remote therapy has already helped many get through this uniquely challenging year.
“We were all focused on Destiny’s wellbeing, and words can’t describe the complete turnaround that she has achieved,” Lewis said. “It’s beyond words and emotions; Abby is like another mother to her now.”

